The following recommendations rely entirely on the guidelines as published by the CDC or OSHA. The OSHA guidelines at www.osha.gov/covid-19/controlprevention.html.
Defining the Risk
In general, we can easily state that response to any potential or confirmed COVID-19 exposure is dependent on several factors including:
- How close the exposure was: CDC defines “close contact” as within six feet or any unprotected direct contact or direct exposure to potentially infectious secretions or indirect exposure (coughing, sneezing)
- Length of exposure: CDC roughly defines the length of exposure to be anything over a few minutes
- Degree of exposure: Exposure to patients with a confirmed diagnosis and/or exhibiting marked signs or symptoms (fever, coughing) increase degree
- Protection during exposure (PPE): Use of recommended PPE by healthcare provide AND patient directly related to the level of risk or exposure
With this in mind, for most eye care encounters utilizing PPE (mainly masks) in the care of patients utilizing PPE (mainly masks), the healthcare worker would be classified in a low-risk category. OSHA has a slightly different risk classification system that places most healthcare providers in a medium risk category but the recommendations for management are similar to the CDC low-risk classification. An exception could be a higher risk when performing procedures that have the potential for aerosol generation (MGD expressions or other gland manipulation – although this risk is minuscule with proper precautions). It could also be considered advisable to delay these kinds of procedures. More information on the degree of risk can be found in the CDC reference.
Despite the fact routine types of optometric care performed on patients with no identified or confirmed risk of exposure the disease poses a very low risk for exposure to COVID-19, this does not remove any recommendation to reduce the risk of disease transmission through social distancing, office disinfection, frequent hand washing and use of PPE (mainly masks).
Response to Potential Exposure
CDC and OSHA both provide guidelines for response to suspect or confirmed individuals with COVID-19 including patients and healthcare workers. We will address each of those groups separately.
For healthcare workers (doctors and staff), the following table, condensed from CDC data, summarizes the correct response to on the job potential or confirmed exposure to COVID-19.
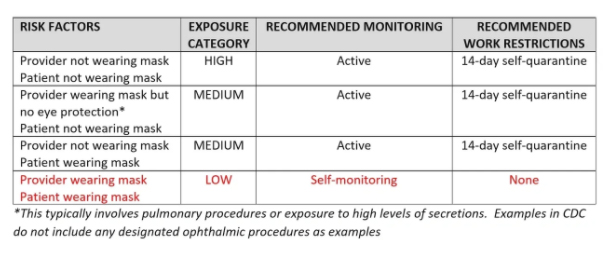
From this table, it is easy to conclude that mandatory wear of masks by both the provider and patient significantly reduces the risk of infection, even in a patient with a suspect or confirmed diagnosis of COVID-19. It is also important to note that not wearing gloves, gowns, or shields in routine encounters does not significantly increase the degree/risk of exposure. Any protections beyond those listed in the table may be excellent precautions but are not included in the CDC mandates.
In addition to the recommendations in the table, the CDC recommends that any planned exposure (treatment) to a patient with confirmed, active COVID-19 should include the following precautions:
- Facemask
- Gown
- Gloves
- Eye protection
One could argue why, except in some sight-threatening situations, ophthalmic care for a confirmed COVID-19 patient would be deemed essential or could not be delayed for a period of time.
Some additional explanation is helpful.
What constitutes a potential exposure? Potential exposure is direct or close contact with an individual who has a confirmed COVID-19 test or is waiting for testing or the results of testing (a person under investigation or PUI). It is NOT every patient that walks into your office. The patient must be directed to immediately report the results of the testing. If no report is made within 72 hours, the provider should consider the PUI (a person under investigation) as a confirmed case. Although not specifically listed in the guidelines, it is also wise to consider any individual with fever (over 100.00) or symptoms consistent with COVID-19 (cough, shortness of breath, sore throat, malaise) as a potential exposure.
What is Active Monitoring? Active monitoring is checking temperature twice daily (looking for fever above 100.00) and/or development of symptoms consistent with COVID-19 (cough, shortness of breath, sore throat, malaise). If fever or symptoms develop, the individual should self-isolate and seek consultation with their general health care provider.
What is Self-Monitoring? Self-monitoring has exactly the same requirements of active monitoring except there are no requirements to consult for care with another healthcare provider or work restrictions imposed unless fever or symptoms develop.
Managing the Confirmed or Suspect Infection in the Office
Whether a patient or healthcare worker, the following should be initiated with any individual suspected of having COVID-19.
- Isolate the individual to a place with the least amount of contact with other patients or healthcare workers
- If the individual does not already have a mask, provide them with one
- Restrict the number of individuals entering the confined area
- Assist the individual with contacting for medical care – removing them from the office as quickly as possible
With the rare exception of some sight or life-threatening presentation, care can be delayed until the potential for disease is either confirmed or removed by testing. There would be no reason to have any patient or healthcare provider remain in the office if they become a PUI.
Office disinfection procedures must be evaluated. General guidelines include: where possible, not using rooms the PUI occupied for 24 hours; thorough disinfection of all areas where the PUI was in contact; and, use of HEPA or similar filtration or at a minimum increase air circulation in the areas. While some have cited mass disinfection and office closure requirements, there are no regulations requiring special sterilization systems, professional disinfection, or office closures for healthcare facilities.
When Can the Healthcare PUI (Person Under Investigation) Return to Work
CDC provides specific guidelines on when individuals suspected or confirmed to be infected with COVID-19 may return to work. The directives fall into four categories and can be viewed as minimal recommendations.
Suspect or confirmed diagnosis based on symptoms
- At least 72 hours have past since recovery defined as absence of fever without fever-reducing medications and improvement in symptoms; AND
- At least 10 days have passed since the onset of symptoms
Suspect or confirmed diagnosis based on testing
- Resolution of fever without the use of fever-reducing medications, AND
- Improvement in respiratory symptoms, AND
- Negative results for COVID-19 – two tests collected > 24 hours apart
Asymptomatic individuals with a positive COVID-19 test based on time strategy
- 10 days have passed since the positive COVID test finding and the individual still has no symptoms
Asymptomatic individuals with a positive COVID-19 test based on test strategy
- Negative results for COVID-19 – two tests collected > 24 hours apart
Once any of these individuals return to work, continuous wear of masks and self-monitoring are essential.
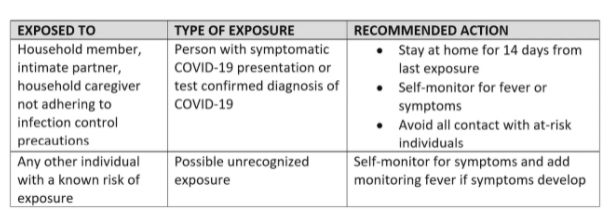
Community Exposure
Community exposure involves a health care provider (doctor or staff) who has off the job exposure to a potential or confirmed COVID-19 individual. This could be contact with a spouse, child, friend, or anyone who reports they have potential or confirmed disease. The following table summarizes the recommended action when a healthcare worker reports potential or confirmed community exposure to COVID-19.