Not many providers understand MIPS and few ODs chose to participate in MIPS, but we do get questions about it frequently. If you are wondering how it applies to you, this article should help.
Does MIPS apply to you?
MIPS does apply to optometrist who bill Medicare and generally exceed the low-volume threshold during the MIPS Determination Period (Oct 1 to Sept 30). The low-volume threshold includes 3 aspects of covered professional services:
- Allowed charges
- Number of Medicare patients who receive covered professional services
- Number of services provided
You must participate in MIPS (unless otherwise exempt) if, in both 12-month segments of the MIPS Determination Period, you:
- Bill more than $90,000 for Medicare Part B covered professional services, and
- See more than 200 Medicare Part B patients, and;
- Provide more than 200 covered professional services to Medicare Part B patients.
If you don’t think you meet the minimum threshold, feel free to stop reading now. If you want to be sure, you can double check your eligibility status here: Participation Lookup (cms.gov). If you think you exceed the minimum threshold, the rest of this article applies to you.
Quality Payment Program (MIPS) Overview
Prior to the launch of the Quality Payment Program (QPP) on January 1, 2017, payment increases for Medicare services were set by the Sustainable Growth Rate (SGR) law. However, as clinicians increased their utilization of services, the reimbursement for each unit of service had to be adjusted downward to hold costs constant. In practice, the SGR would have resulted in large decreases in the Physician Fee Schedule, which wasn’t sustainable. To avoid these decreases in reimbursement, Congress had to pass a new law (every year) authorizing the current fee schedule and a small increase for inflation.
With the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), CMS discontinued the use of the SGR as a basis for clinician payments. QPP gave CMS the ability to reward high-value, high-quality Medicare clinicians with payment increases – while at the same time reducing payments to those clinicians who weren’t meeting performance standards. The program established a model of funding that rewards clinicians who provide high-quality patient-centered care. QPP attempts to improve the quality and safety of care for all individuals and to reduce the administrative burden on clinicians, whether it actually accomplishes this or just increases the difficulty of filing claims remains to be seen.
Traditional MIPS Requirements
MIPS grades the “quality” of care provided based on 4 measures:
- Quality – based on performance measures created by CMS. You pick the quality measures that best fit your practice. They easiest and most common way to report them is by adding additional codes to your claims to report what you did.
- Promoting Interoperability – promotes patient engagement and the electronic exchange of health information using certified electronic health record technology (CEHRT). You report a defined set of Promoting Interoperability objectives and measures. This is very similar to how Meaningful use worked and is essentially the new version of Meaningful Use.
- Improvement Activities – assesses how you improve your care processes, enhance patient engagement in care, and increase access to care. You choose the activities appropriate to your practice. You start the activities during the
- Cost – assesses the cost of the patient care you provide. CMS calculate cost measures, based on your Medicare claims, to determine the cost of the care you provide to certain patients.
MIPS Scoring
Each of these activities are graded at the end of the reporting period (calendar year) and a total grade on a scale of 0 to 100 is given based on the sum of the scores in each area:
- Quality 30%
- Promoting Interoperability 25%
- Improvement Activities 15%
- Cost 30%
Getting started:
As you can see from the scoring above, 60% of the MIPS score is based on Quality measures and Cost. Cost is calculated automatically (you don’t have to do anything) and Quality measures can be easily (or at least somewhat easily) reported on your Medicare claims. For that reason, we generally recommend starting by adding the appropriate quality codes to your claims. By doing that you could get at least 60 points (30 from Quality and 30 from cost) and potentially avoid a penalty altogether. So let’s take a look at what you need to do to participate and in and report MIPS Quality measures.
1. MIPS Quality Measure Data
You must collect measure data for the 12-month performance period (January 1 – December 31). There are 5 collection types for MIPS quality measures:
- Electronic Clinical Quality Measures (eCQMs);
- MIPS Clinical Quality Measures (CQMs);
- Qualified Clinical Data Registry (QCDR) Measures;
- Medicare Part B Claims Measures; and
- The Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS Survey.
General reporting requirements are that you need to submit collected data for at least 6 quality measures (including one outcome measure or high priority measure in the absence of an applicable outcome measure), or a complete specialty measure set. You’ll need to report performance data for at least 70% of the denominator eligible cases for each quality measure (data completeness). You can submit measures from different collection types to fulfill the requirement to report data for at least 6 quality measures.
You can explore the full list of CMS quality measures here. But in simple terms, for certain diseases (ICD codes) you can add a special procedure code (CPT code) to the claim to indicate to CMS that you provided quality care in that circumstance. The AOA also has a great document that summarizes which MIPS measures apply to optometry. The measure that would apply to optometry include the following measure numbers:
- 1 (NQF 0059) Diabetes: Hemoglobin A1c (HbA1c)
- 128 Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow-Up Plan
- 141 (NQF 0563) Primary Open-Angle Glaucoma (POAG): Reduction of Intraocular Pressure by 15% OR Documentation of a Plan of Care
- 155 (NQF 0101) Falls: Plan of Care
- 226 (NQF 0028) Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
- 236 Controlling High Blood Pressure
- 317 Preventive Care and Screening: Screening for High Blood Pressure and Follow-Up Documented
Once you have gotten comfortable with adding the MIPS Quality measures codes to your claims, you can move on and deal with the Promoting Interoperability and Improvement Activities.
2. Promoting Interoperability
The Promoting Interoperability performance category promotes patient engagement and electronic exchange of information using certified electronic health record technology (CEHRT).
For each performance year, you’re required to use an Electronic Health Record (EHR) that meets the 2015 Edition Cures Update certification criteria for participation in this performance category.
You must submit collected data for the required measures in each objective (unless an applicable exclusion is claimed) for the same 90 continuous days (or more) during 2023.
In addition to submitting measures, you must provide your EHR’s CMS identification code from the Certified Health IT Product List (CHPL) and submit a “yes” to:
- The Actions to Limit or Restrict Compatibility or Interoperability of CEHRT (previously named the Prevention of Information Blocking) Attestation.
- The Office of the National Coordinator for Health Information Technology (ONC) Direct Review Attestation.
- The Security Risk Analysis Measure.
- The Safety Assurance Factors for EHR Resilience (SAFER) Guides Measure (a “no” will also satisfy this measure).
There are 3 ways that you can report Promoting Interoperability performance category data. The 3 options are:
- Sign in and attest
- Sign in and upload
- Direct submission via Application Programming Interface (API)
Most optometrist choose the 1st option.
Scoring can be a little complicated for the Promoting Interoperability measures, but CMS does the calculations for you based on your reporting.
3. Improvement Activities
The improvement activities performance category measures participation in activities that improve clinical practice
To earn full credit in this performance category, you must generally submit one of the following combinations of activities:
- 2 high-weighted activities,
- 1 high-weighted activity and 2 medium-weighted activities, or
- 4 medium-weighted activities.
Improvement activities have a minimum of a continuous 90-day performance period (during calendar year (CY) unless otherwise stated in the activity description. Each activity must be performed in the CY, but multiple activities don’t have to be performed during the same 90-day, or otherwise specified, period.
As with Promoting Interoperability there 3 ways to report improvement activities, The options are:
- Sign in and attest
- Sign in and upload
- Direct submission via Application Programming Interface (API)
As with Promoting Interoperability, most optometrist choose the 1st option.
High-weighted activities receive 20 points and medium-weighted activities receive 10 points. There is a maximum of 40 points that can be earned from attesting to activities in this performance category.
4. Cost
Medicare uses administrative claims data to calculate cost-measure performance, which means you don’t have to submit any data for this performance category.
You’ll be evaluated and scored on each cost measure for which you meet or exceed the established case minimum. Medicare determines measure achievement points by comparing performance on a measure to a performance period benchmark.
Putting it all together
As previously stated, each of these activities are graded at the end of the reporting period (calendar year) and a total grade on a scale of 0 to 100 is given based on the sum of the scores in each area:
- Quality 30%
- Promoting Interoperability 25%
- Improvement Activities 15%
- Cost 30%
Payment Adjustments
This table shows how your score then affects your payment in the following year:
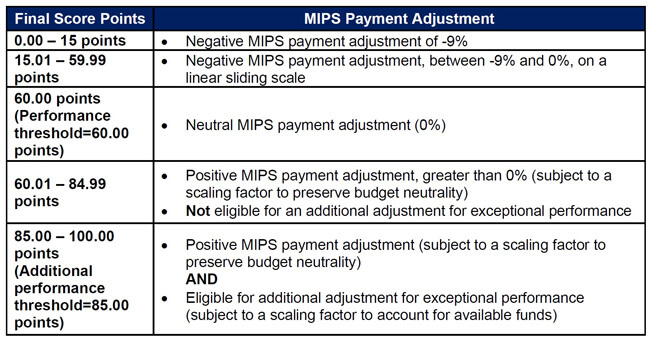
So, as you can see, you could potentially have your Medicare payments reduced by as much as 9% if you receive a low score (or if you are not submitting data). For optometrists who bill a significant amount to Medicare, it could be quite costly to ignore MIPS.
As always feel free to reach out at info@practicecompliancesolutions.com with any questions you might have.
– The PCS team